
A New Synthetic Simulation of Kidney Filtration
With a focus on macromolecular purification
WRITTEN BY ANTONIO ESHO
ILLUSTRATED BY ANDREA ARMENDI
Introduction
Kidneys are the workhorse of the renal system and facilitate filtration of nutrients and waste, and maintenance of body fluid levels in the blood. Utilizing blood pressure, the kidneys squeeze water, ions, and waste materials like urea out of the blood, excreting the waste through urine. They then reabsorb needed substances like sodium, potassium, and glucose back into circulation.
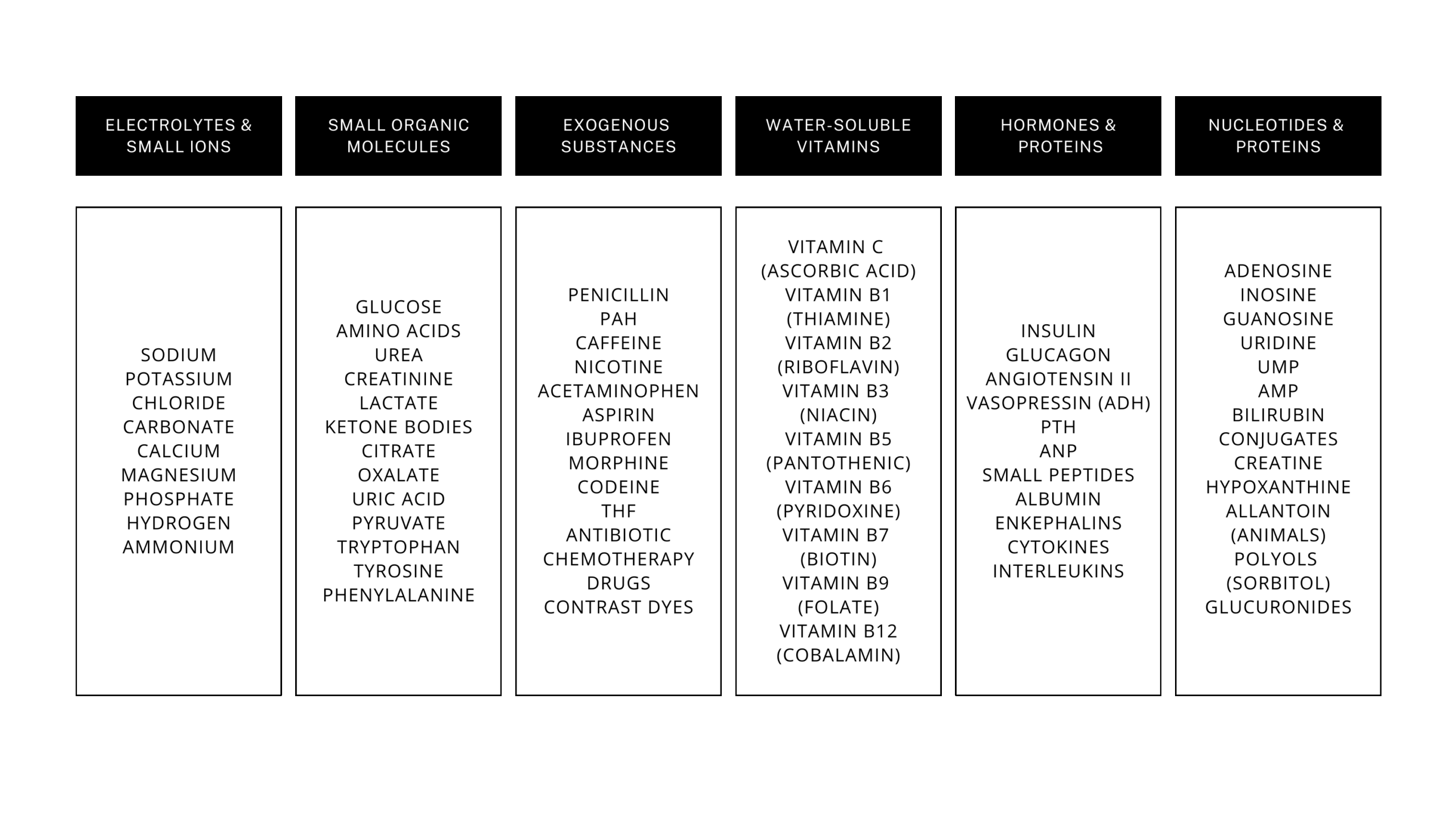
Blood primarily consists of water-like plasma and blood cells. The kidney’s general functionality involves connecting blood vessels to a glomerular filter that pushes all particles out of the blood and into the kidney. Inside, all of the filtered substances are reabsorbed into the blood circulation using concentrations of the individual solutes. This process is extremely complicated because of the slew of different molecules that need to be reabsorbed, as shown in Table 1.
Kidneys use chemical equilibrium properties to take advantage of blood direction and pressure for filtration of materials out of the blood. However, due to growing changes in diet and the rise of diabetic stressors that limit the ability to pull glucose out of the blood, Chronic Kidney Disease (CKD), or the long-term lack of kidney function is growing in the general population.1 Diabetes-mediated high glucose levels damage the kidneys through added filtration pressure on the kidneys over time. Diabetes puts stress on the kidneys and increases the likelihood of undue kidney filtration and reabsorption from decreasing kidney functionality over time, amplifying the onset of CKD.
Synthetic approaches are needed in order to offload the responsibility of filtering blood off of the kidneys to reduce symptoms of CKD. This artificial process of kidney filtration can be reestablished in order to simulate kidney function in the human body and reestablish nutrient equilibrium.
Methods
The rise of CKD summons a rising interest in artificial simulations of kidney function to improve the quality of life of patients with the condition. Two current forms of treatment for CKD include peritoneal dialysis and hemodialysis.
Peritoneal Dialysis
Peritoneal dialysis involves filling the peritoneum, the tissue lining around organs, with a high osmolarity dialysis solution. This draws fluids out of the body into the peritoneum lining, then drains the peritoneal cavity to remove the excess fluids and solutes out of the body that the kidney cannot fully filter, as visualized in Figure 1. This process is repeated to draw excess fluid and solutes out of the body to supplement the long-term lack of kidney function in CKD (NIDDK).

Hemodialysis
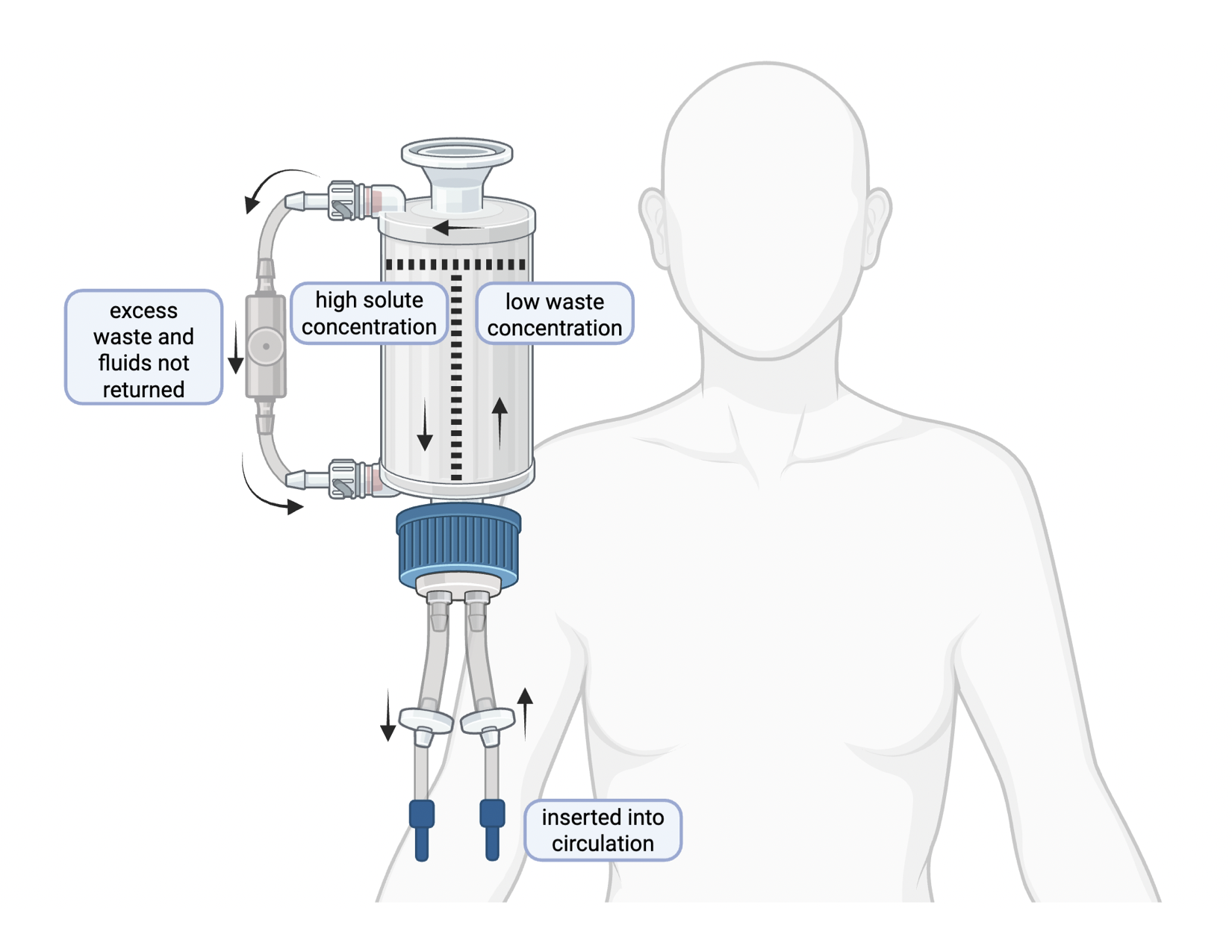
Alternatively, hemodialysis connects blood circulation to an external filtration compartment with a semipermeable membrane to allow fluid and solutes to diffuse out of the blood. Concentration gradients are then applied to solutes like glucose, sodium, and others in Table 1, which are returned to the body. Any extra fluid, solutes, and waste products that dissolved out of the blood into the dialysis fluid mixture can be siphoned out of the body. Filtered blood is then returned to the circulation to ease the load on the kidney.

Each filtration technique requires surgery to insert catheters into the body for facilitated access to the circulation in dialysis clinics. Additionally, both make it more difficult to maintain body temperature. Peritoneal dialysis repeatedly pumps water into the body’s core, while hemodialysis pulls blood out of the body, where it cools before returning into circulation. Additionally, 10-15 hours are spent in the dialysis clinics waiting for the dialysis machine to filter the blood. These deficits severely impact the quality of life of people with CKD.
Conclusion
Kidneys filter out all materials in the blood, except for blood cells and large proteins like albumin that cannot enter the kidney nephrons. A substitution for kidneys must include a large scale and variable filtration of blood products. Therefore, a synthetic kidney functionality must involve non-discriminatory excretion of materials, then the selective reabsorption of needed solutes, like potassium, calcium, and glucose.
This conclusion involves the selective removal of waste products and excess fluid in order to circumvent the limitation of a two-directional flowing of materials out of and back into circulation that does not efficiently remove certain materials out of the blood, like waste products. A possibility to increase the efficiency of dialysis would be to mimic true kidney filtration by separating blood circulation into two individual processes. First, a secretion phase where all solutes and wastes are excreted, followed by a second step where solutes are reabsorbed into the circulatory system after the filter has selectively removed waste products. This is done in order to intentionally control the direction of solute movement rather than removing all solutes and fluids without discrimination like the previously mentioned dialysis techniques. A possible design of this medical device is shown in Figure 3.
This synthetic production can be simulated in a bi-compartmental medical device that isolates the excretion of materials and reabsorption of needed materials. Therefore, instead of previous processes involving the less discriminatory removal of solutes and waste products with excess fluids, a more streamlined approach would isolate each process, filtration and reabsorption to be more analogous to in vivo kidney function.
Because they filter out all materials in blood, kidney functionality must be extrapolated. Synthetic approaches to blood filtration and liquid excretion have been developed, and will continue to be iterated upon to improve functionality for patients with reduced renal capability, such as those with CKD.
References
- Katella, Kathy. “Why Is Chronic Kidney Disease (CKD) on the Rise? 6 Things to Know.” Yale Medicine, 24 Apr. 2024, www.yalemedicine.org/news/why-is-chronic-kidney-disease-ckd-on-the-rise.
- “Peritoneal Dialysis | NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases, www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/peritoneal-dialysis#prepare.
- National Kidney Foundation. “Hemodialysis.” National Kidney Foundation, 12 Aug. 2024, www.kidney.org/kidney-topics/hemodialysis.
- National Institute of Diabetes and Digestive and Kidney Diseases. “Hemodialysis.” National Institute of Diabetes and Digestive and Kidney Diseases, Jan. 2018, www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis.
